Your PBM Profits From Complexity. You Pay for It.
Fiduciary pharmacy benefits administration that removes conflicts, simplifies the model, and holds us contractually accountable to employer outcomes.

Pharmacy Benefit Administration (PBA)
Claims adjudication, eligibility, plan configuration, prior authorization administration, and reporting with radical transparency. Employers, brokers, and TPAs gain control, predictability, and lower pharmacy spend while members get a smoother, more reliable experience.
Reduce spread pricing, regain control of rebates, and eliminate plan leakage.
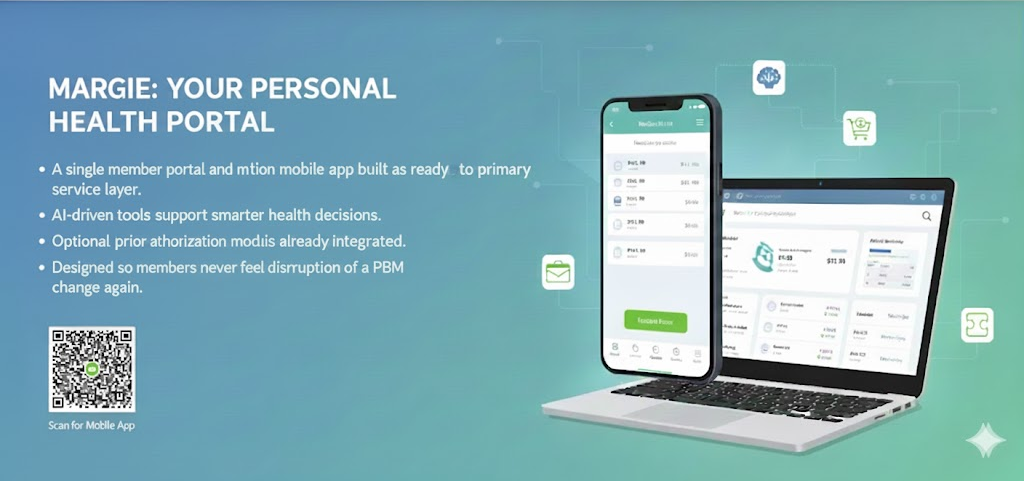
Member Portal and Mobile Application
A single member portal and mobile app built as the primary service layer. AI-driven tools support smarter decisions, optional built-in prior authorization reduces friction, and Mark Cuban Cost Plus Drugs is already integrated. Designed so members never feel the disruption of a PBM change again.
Speeds decisions, improves outcomes, and lowers costs through fiduciary oversight.
InsourceRx Analytics
Self-service dashboards for Rx and J-code claims. Built for finance, HR, and advisors. White-label and self-hosted options keep personally identifiable information and protected health information securely within your environment.
Back fiduciary decisions with on-demand, defensible insights.
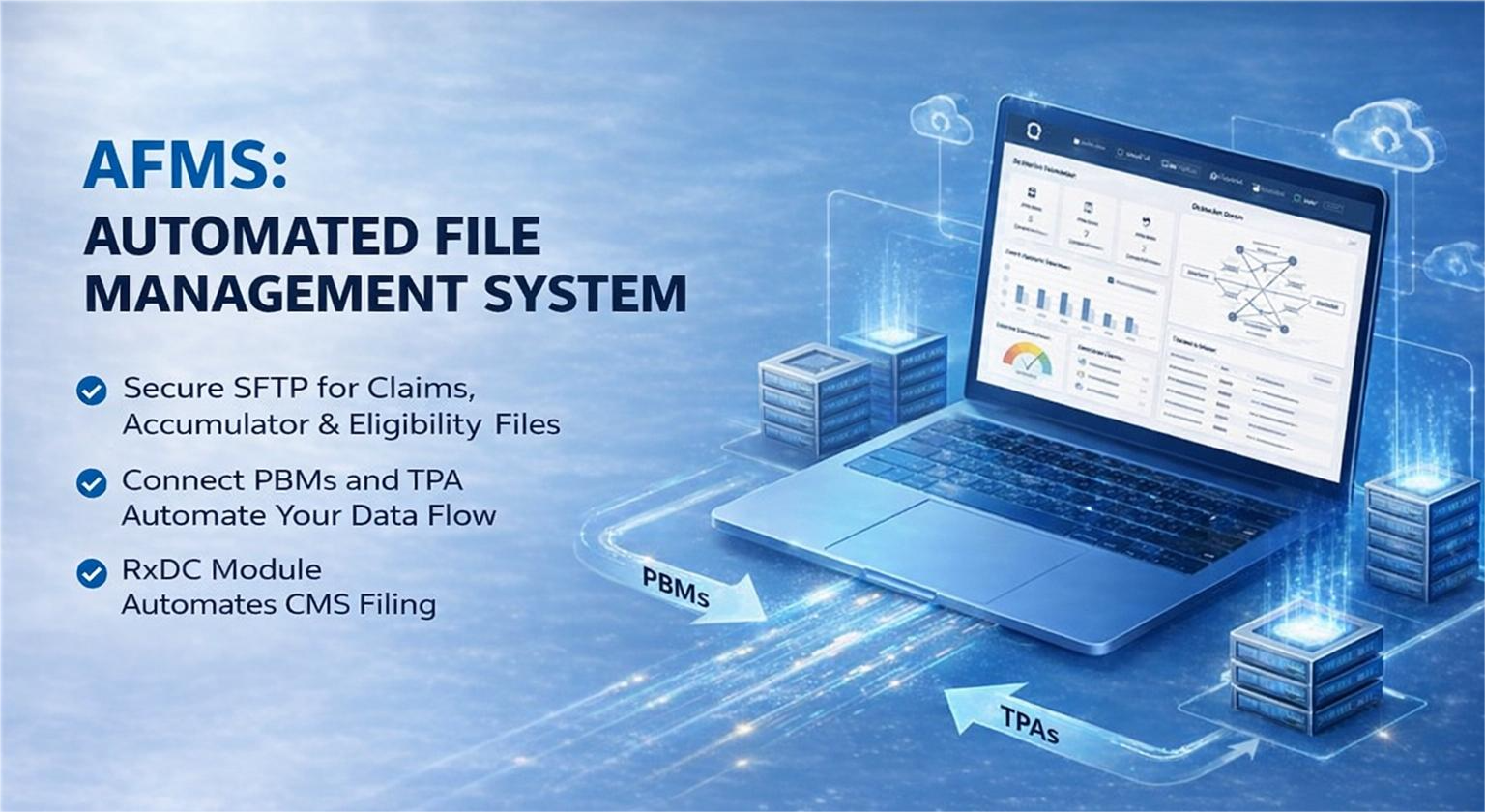
RxDC Reporting Software
Automates CMS RxDC filing by syncing PBM, TPA, and employer data.
Avoid penalties, maintain compliance, and preserve trust.
Automated File Management System (AFMS)
Connect PBMs and TPAs via secure, automated SFTP for claims, accumulators, and eligibility data.
Improves accuracy, reduces manual labor, and enforces data integrity.
Specialty Drug Management
Purpose-built program to manage high-cost drugs and improve adherence.
Gain full cost visibility and eliminate markup games.
Formulary and Utilization Management
Step therapy, QLs, and clinical rules across both benefits, seamlessly enforced.
Defend your plan with appropriate use, not overuse.
Built for Fiduciaries
Every solution is purpose-built to uphold your fiduciary duty by minimizing conflicts of interest
and protecting plan assets with radical transparency.